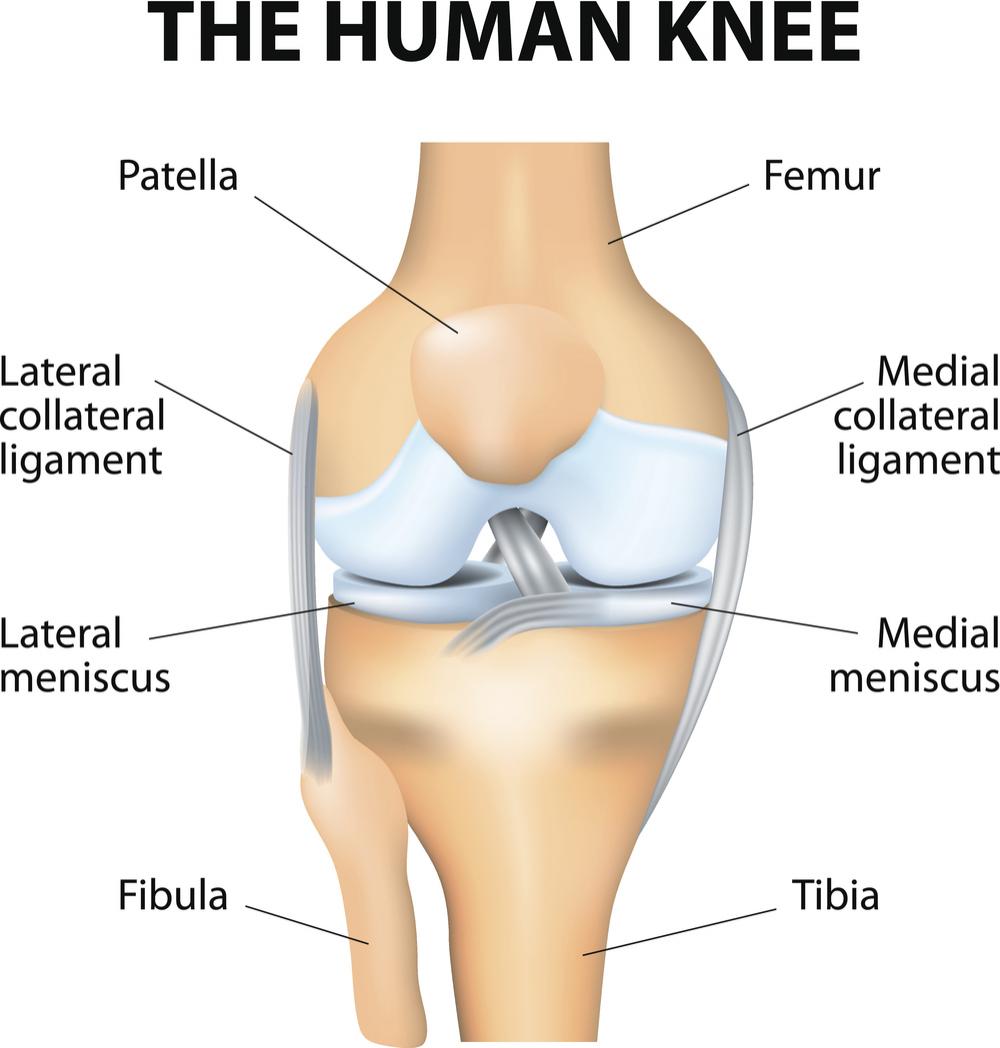
Anatomy of Knee
The bones of the knee, the femur and the tibia, meet to form a hinge joint. The joint is protected in front by the patella (kneecap). The knee joint is cushioned by articular cartilage that covers the ends of the tibia and femur, as well as the underside of the patella. The lateral meniscus and medial meniscus are pads of cartilage that further cushion the joint, acting as shock absorbers between the bones.
Ligaments help to stabilize the knee. The collateral ligaments run along
the sides of the knee and limit sideways motion. The anterior cruciate
ligament, or ACL, connects the tibia to the femur at the center of the
knee. Its function is to limit rotation and forward motion of the tibia.
(A damaged ACL is replaced in a procedure known as an ACL Reconstruction.)
The posterior cruciate ligament, or PCL (located just behind the ACL)
limits backward motion of the tibia.
These components of your knee, along with the muscles of your leg, work together to manage the stress your knee receives as you walk, run and jump.
Cartilage Repair
Injured Cartilage
A severe knee cartilage injury can radically change an active adult's lifestyle. Symptoms such as locking, catching localized pain and swelling often affect your ability to work, play, and even perform normal activities.
A cartilage lesion appears as a hole or divot in the cartilage surface. Since cartilage has minimal ability to repair itself, even what may seem like a small lesion (ranging from the size of a dime to a quarter), if left untreated, can hinder your ability to move free from pain, and cause deterioration to the joint surface.
Treatment with Autologous Chondrocyte Implantation (ACI)
Although cartilage is unable to repair itself on its own, advanced FDA-approved technology allows cartilage cells, known as chondrocytes to be harvested from your knee and cultured and multiplied. The fresh chondrocytes are then re-implanted in your knee and cause hyaline cartilage to regenerate. This biological repair is known as ACI. When you successfully complete ACI and rehabilitation, you should be able to resume all normal activities, including sports.
ACI, also known as Carticel treatment, restores the articular surface and regenerates hyaline cartilage without compromising the integrity of healthy tissue or the subchondral bone. Carticel has demonstrated important benefits in patients with a type of lesion called a femoral focal lesion. If your orthopedic surgeon has determined that you have this type of lesion, then Carticel may be an appropriate treatment option. The procedure consists of two steps. The first is the harvesting of some healthy cartilage from your knee through an arthroscope. This sample of cartilage is used to create new chondrocytes, which take 3-4 weeks that are then re-implanted in your knee. The second step is the reimplantation of the cultured chondrocytes, or Carticel. This procedure is done through an arthrotomy, and is depicted below.
Implantation of Carticel:
- Step 1: An arthroscopic biopsy - First, the surgeon examines your knee through an arthroscope - a small device that allows the doctor to see into your knee joint. If a lesion is detected, a tiny biopsy of healthy cartilage tissue will be removed.
- Step 2: Cell culture processing - The cartilage sample is then sent to Genyzme Tissue Repair (GTR), where it is cultured. Cell culturing takes about 4-5 weeks, during which time your cells multiply significantly. About 12 million cells will be supplied to your surgeon at the time of your operation.
- Step 3: A surgical procedure is performed, and the damaged cartilage is removed.
- Step 4: Periosteum, skin that covers the bone, is sutured over the prepared defect.
- Step 5: Surgical implantation - The cultured cells are then implanted into the lesion. Here, the cells may continue to multiply and integrate with surrounding cartilage. With time, the cells will mature and fill-in the lesion with hyaline cartilage.
Post-Operative Rehabilitation
To derive maximum benefit from ACI, you should adhere strictly to the personalized rehabilitation plan recommended by your physician. This will include progressive weight-bearing, range of motion, and muscle strengthening exercises which may begin as early as the day after surgery.
